
Pericoronitis
Pericoronitis
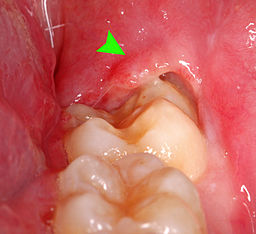
Pericoronitis is an acute infection with inflammation of surrounding safe tissues of the partially erupted impacted tooth. When the third molar (Wisdom tooth) fails to erupt completely incorrect position will pave the way for pericoronitis. But it can occur around the base of any tooth that is more common in the third molar and mostly evidenced in late adolescence (20-30yrs of age).
Pericoronitis is of two types. Acute pericoronitis have severe symptoms, systemic involvement. Acute pericoronitis is seen in patients with poor oral hygiene. Chronic pericoronitis have mild symptoms and seen in patients with moderate oral hygiene.
Causes:
Pericoronitis is caused by multiple facultative anaerobic bacteria which are peptostreptococcus, fusobacterium, and Bacteroides. When the tooth partially erupts it will be associated with soft tissue covering the tooth partially which is called the operculum. Third molars are located at the back of the mouth. So it makes it difficult to achieve effective cleaning while brushing. Impaction in this region will be high which becomes the favorite place for bacteria to grow and multiply.
Initially the overlapped tissue (operculion) inflame if not treated infection may spread to adjacent tissues and worsen the condition. Supra erupted upper third molar can cause constant trauma to the operculum and aggravate the situation. On the inner surface of the operculum, there are various degrees of ulceration.
Signs and symptoms:
- 1.Pain
- 2.Redness
- 3.Swelling of tissue
- 4.Difficulty in chewing
- 5.Difficulty in opening the mouth
- 6.Increase in body temperature
- 7.Pain may radiate to other parts like the ear, throat, the floor of the mouth.
- 8.Halitosis (bad breath)
- 9.Pus discharge
- 10.Bad taste in the mouth
- 11.Extraoral swelling (i.e., angle of mandible)
- 12.Lymphadenopathy
- 13.Inability to close the jaw
- 14.Loss of appetite
- 15.Fatigue
- 16.Leucocytosis
If pericoronitis is not treated may lead to complications. Pericoronitis convert into pericoronal abscess and may spread posteriorly into the oropharynx and to the base of the tongue leads to difficulty in swallowing. Then it causes space infection. The sequel of acute pericoronitis is peritonsillar abscess formation, cellulitis. Ludwig's angina. It requires hospitalization and can be a life-threatening situation.
Treatment for Pericoronitis
Treatment of pericoronitis depends on the severity of the inflammation and systemic complication.
1.The inflamed region is irrigated with warm water or chlorhexidine solution to remove debris and exudates (pus).
2.The inflamed flap is deflated and cleaned with a scalar.
3.If pericoronitis flap is traumatized by opposing tooth, then the inflamed flap is removed or occlusal adjustment is done.
4. In pericoronitis with system conditions, antibiotics and analgesics are prescribed.
5. 0.12% chlorhexidine mouthwash or warm water rinse twice a day is advised.
6. If the tooth is erupting in the proper position, then the inflamed pericoronil flap is removed which is called operculectomy. This procedure is done to retain the function of the tooth.
7. If the tooth impacted or recurrent infection occurred then extraction is the choice of treatment.
8. Good oral hygiene maintenance and regular follow-up is suggested.

Author: Dr. M. Jovitta, Pediatric /Preventive Dental Health Expert,
Jerush Dental & Facial Corrective Centre
Click to read Dr. Jovitta's other blogs: "Why flossing is important" "Brushing Techniques" "Bad breath or Halitosis" "Smoking and Oral Health", Tooth replacement options for missing teeth" "Dental pain & Root canal Procedure", "Coronavirus (COVID-19), Symptoms and Prevention", "Gingivitis & Covid 19" "Oral cancer treatment"

No Comments yet!