
The tongue is a group of muscles that helps for tasting swallowing, speaking, etc. The surface of the tongue is covered by small bumps called papillae. Taste buds are present in papillae. The tip of the tongue is more sensitive to sweetness, both sides of the tongue to sour taste and back of the tongue to bitter taste. Salt taste sense is widely spread in the tongue. But it is greatest in the tip. The tongue is mobile and firmly attached to the floor of the mouth. The tongue is affected by oral disease and shows signs of other systemic diseases. So it is important to inspect the tongue regularly and take care of it.
Signs of disease in tongue:
Candidiases or Oral thrush!
Candidiasis is caused by a yeast-like fungus called conidia albicans. It is the most common disease in the tongue. It appears as most white patches. For infants, candidiasis is painless but for adults, causes a burning sensation. It is most common in women. Oral candidiasis is caused by poor oral hygiene maintenance and other systemic conditions like AIDS, Immunosuppression, diabetes, drugs et. Oral candidiasis is easy to wipe out with gauze. Persistent causative organism leaves ulcerative painful red lesions upon the removal of white patches. A topical anesthetic gel is given pain a burning sensation.
Leukoplakia
It is also called chronic superficial glossitis. It is caused by syphilis, smoking, sharp tooth, sepsis, spices, Leukoplakia affect anterior 2/3rd of the tongue. The affected area of the tongue shows a white patch with fissures and cracks. Treating the symptom and removing the causative is the treatment for leukoplakia.
Squamous cell carcinoma:
Squamous cell carcinoma is the most common carcinoma in the tongue. It is caused due to chronic dental trauma, tobacco smoking, candidiasis, syphilis, trauma, alcohol. The common sign of carcinoma in tongue is painless ulceration, excessive salivation, sore throat, difficult to speak, hoarseness of voice and difficult to swallow. The affected tongue is treated according to the severity.
Aphthous ulcer:
Aphthous ulcer is a painful single or multiple ulceration. This ulcer is recurrent and heals spontaneously. Aphthous ulcer is due to stress, vitamin B12, folic acid, and iron deficiency, allergy and after cessation of smoking, streptococcus sanguinis and 2 hemolytic streptococcus are causative organisms. The aphthous ulcers can be healed in 7-10 days. For treatment, vitamin supplements is prescribed and topical anesthesia to reduce pain.
Glossitis:
In iron deficiency, anemia the tongue appears smooth, glazed, fiery red, swollen, and painful tongue. It is also associated with disturbed taste and dry mouth. For treatment, iron supplements are prescribed.
Geographic Tongue:
Geographic tongue is an irregular reddish area, surrounded by white papillae. It is associated with psoriasis and lichen planus. It increases sensitivity towards spices sweet and salt. This lesion heals and recurs in other parts of the tongue. It causes pain or a burning sensation. Topical corticosteroids, topical anesthesia are given to subside symptoms. Zinc supplements and a bland diet are advised.
Black hairy tongue:
A black hairy tongue is the overgrowth of papillae of the tongue with an accumulation of keratin. It is caused by poor oral hygiene, fungal infection, bacterial overgrowth, radiation, use of drugs like penicillin, sodium peroxide. Increased length of papilla brushes and the palate cause gagging. Brushing the tongue for 2 minutes twice daily is advised. Topical agent podophyllum is prescribed.
How to clean tongue:
Tongue scraping:
Tongue scraping is used to remove debris from the surface of the tongue. The volatile sulfur compound (odor-causing substance) should be scraped off to prevent bad breath. A tongue scraper or toothbrush is used to clean the tongue. Tongue scraping is done after brushing and flossing. The scrapper is placed as far back of the tongue as possible. With gentle pressure, scrape the tongue. Rinse the scraper. Swish the mouth with water. Repeat scrapping. Another equally effective method is brushing the tongue. In this method, the toothbrush is used to clean the tongue. Gently brush the tongue for two minutes daily. These two methods remove harmful bacteria from the tongue.
Conclusion:
Every day in the morning routine while brushing teeth tongue hygiene should not be forgotten. Any changes in the tongue should never ignore. Taking care of the tongue improves taste and reduces bad breath.
 Dr-Jovitta
Dr-Jovitta
Author: Dr M. Jovitta, Pediatric /Preventive Dental Health Expert,
Jerush Dental & Facial Corrective Centre
Click to read Dr Jovitta’s other blogs: “Why flossing is important” “Brushing Techniques” “Bad breath or Halitosis” “Smoking and Oral Health”, Tooth replacement options for missing teeth” “Dental pain & Root canal Procedure”, “Coronavirus (COVID-19), Symptoms and Prevention”, “Gingivitis & Covid 19″ “Oral cancer treatment” “Pericoronitis” “Teething” “Invisalign” “Dental jewels”


 Diabetes Checking @ Jerush
Diabetes Checking @ Jerush

 tooth jewellry -Girl
tooth jewellry -Girl

 Invisalign, The best orthodontic treatment
Invisalign, The best orthodontic treatment

 Teething-Dental Hospital Nagercoil,
Teething-Dental Hospital Nagercoil,

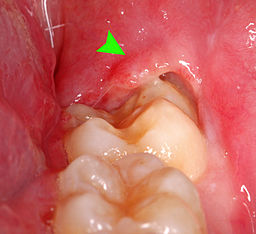 Pericoronitis-Photo
Pericoronitis-Photo

 oral Cancer Treatment in South India
oral Cancer Treatment in South India

 Gum Disease, different stages
Gum Disease, different stages

 1. How to remove facemask. | 2. N95-Mask
1. How to remove facemask. | 2. N95-Mask
 Dr. Aiswarya
Dr. Aiswarya

 Coronavirus Prevention
Coronavirus Prevention

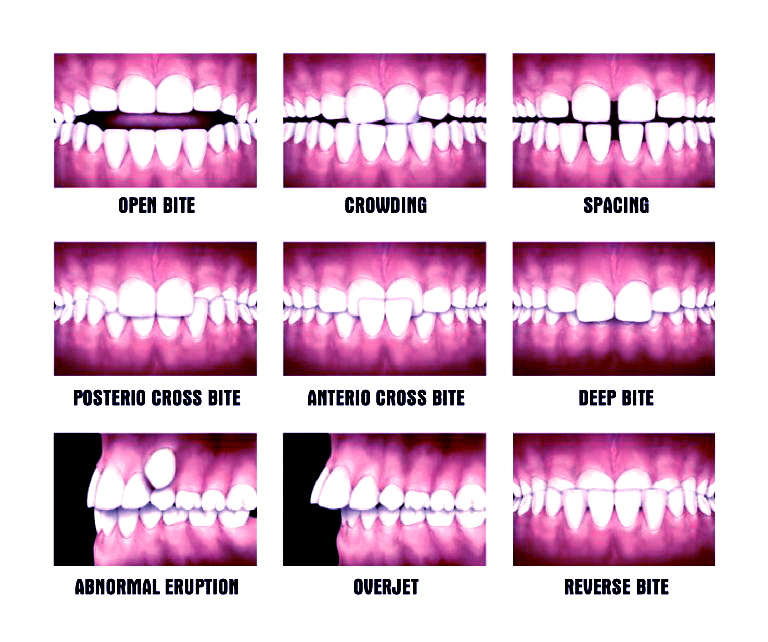 Malocclusion-types
Malocclusion-types
 Dr. Sangari
Dr. Sangari

 Types of dental stains 1. Intrinsic Stain 2. Extrinsic Stain
Types of dental stains 1. Intrinsic Stain 2. Extrinsic Stain